Author: Sun Weiqing
What is global health governance? What changes and challenges does global health governance face? How to strengthen global health governance?
The global health governance structure refers to the organization, mechanism and policy framework for coordinating and managing global health affairs, aiming to respond to global public health challenges, coordinate international cooperation, promote the development of health systems and improve global health conditions. The outbreak of the COVID-19 pandemic in 2019 has caused a setback in the hard-earned global health progress of the past two decades, exposing the shortcomings of the global health system and highlighting a series of challenges facing the global health governance structure.
 (LA Johnson/NPR/Getty/Photo)
(LA Johnson/NPR/Getty/Photo)
Global health governance has gone through four stages
Since the mid-nineteenth century, the development of global health governance has gone through four stages, with topics, goals, participants and tools expanding. The global health governance system has evolved from limited rules formally agreed upon by countries to a complex network involving all countries and numerous non-state actors.
The first stage was the birth of international health cooperation.The first International Sanitary Conference held in Paris, France in 1851 marked the establishment and institutionalization of the international health system. In 1892, the International Sanitary Convention came into force. In the early twentieth century, the first permanent international organizations aimed at promoting international health cooperation, such as the International Office of Public Health (OIHP), were established. After the First World War, the League of Nations International Health Organization (LNHO) was established. These organizations laid the foundation for the establishment of the World Health Organization (WHO).
The second phase saw the birth of the WHO and the heyday of “international” health.In 1948, the WHO and the United Nations system were established after World War II, setting the goal for more ambitious international health cooperation. The WHO's mandate covers a wide range of public health issues. In the following decades, WHO-sponsored projects successfully eradicated smallpox, eliminated malaria in some areas, conducted research on tropical diseases, and launched a campaign to expand primary health care to all. However, in the 1980s, the influence of Cold War ideology led to the decline of the WHO. In the 1990s, the United States froze its core budget support, causing the WHO to fall into a trough. Since then, the search for a new multilateral global health governance model has been put on the agenda.
The third phase was the era of the Millennium Development Goals (MDGs) and the birth of global health.Since the 1990s, all parties have gradually realized that health is an important development, economic and security issue. Three of the Millennium Development Goals are directly related to health, and health has become the core of the global development agenda. With economic development and globalization, the private sector and public-private partnership mechanisms have increased significantly, affecting and changing the structure of the global health governance system. The emergence of many non-state actors, population growth, infectious diseases such as AIDS, and the expansion of political influence in the global South are the characteristics of global health governance at this stage.
The fourth stage is the era of Sustainable Development Goals (SDGs).The Sustainable Development Goals (SDGs) reached in 2015 marked a major change in global health, from the disease-focused Millennium Development Goals to a renewed emphasis on health systems and the more ambitious vision of Sustainable Development Goal 3: "Ensure healthy lives and promote well-being for all at all ages." The world faces many health challenges at this stage, such as the unfinished MDG agenda of HIV, tuberculosis, malaria, maternal and child health, disease outbreaks, non-communicable diseases, aging societies, unsustainable growth in medical spending, and the impact of climate change on health. With the participation of more actors, the diversification of the global health governance process will continue.
Global health institutions are crucial to global health governance
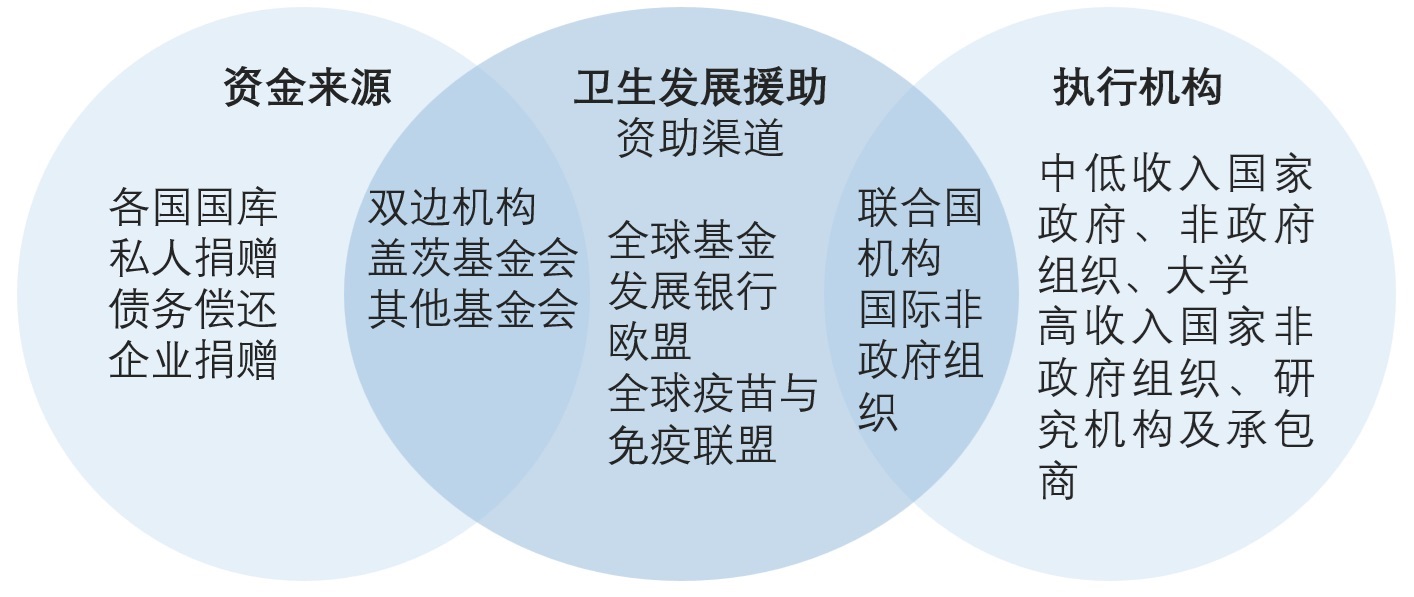
Global health institutions refer to organizations and institutions dedicated to promoting cross-border and cross-regional cooperation to promote the development of global health affairs. These institutions play an important role in global health governance, coordinating international cooperation, promoting policy making and health system development. They also help countries improve health conditions and respond to global health challenges by providing technical support, financial assistance, coordination and cooperation. The public-private partnerships that emerged in the late 20th and early 21st centuries have led to major changes in global health governance. Compared with traditional institutions such as the World Health Organization and the World Bank, which have a wider range of missions and activities, new organizations and vertical funds such as the Global Fund (The Global Fund to Fight AIDS, Tuberculosis and Malaria) and the Global Vaccine Alliance (Gavi) have focused on specific challenges, attracted a lot of financial support, and achieved measurable results.
Global health actors
(Global Health Governance at Crossroads/Photo)
World Health Organization (WHO)It is a professional organization of the United Nations responsible for health affairs and has played an important role in improving global public health. Since its establishment in 1948, WHO has been committed to ensuring that everyone in the world has an equal chance to live a safe and healthy life and promoting important public health achievements around the world. For example, it has promoted the basic eradication of malaria in developed countries and actively prevented and controlled malaria in developing countries. In addition, WHO has promoted the implementation of the global smallpox vaccination program and officially announced the global eradication of smallpox in 1980. The World Health Assembly is the highest decision-making body of WHO, responsible for determining WHO policies, appointing the Director-General, overseeing fiscal policies, and reviewing and approving plans and budgets. The theme of the 77th World Health Assembly in 2024 is: All for Health, Health for All. The main agenda includes reviewing the WHO's General Programme of Work, the Pandemic Agreement and amendments to the International Health Regulations.
United Nations Children's Fund (UNICEF)UNICEF plays an important role in protecting children's health and promoting global public health. UNICEF is committed to protecting children's health and ensuring their health and well-being by providing basic health care, vaccinations, nutritional support and other services. In addition, UNICEF also promotes the solution to global child malnutrition through nutrition projects and policy advocacy, improves children's nutrition levels, promotes hygiene awareness, and provides medical services and basic necessities for children affected by humanitarian crises.

(World Bank/Photo)
World Bank (WBG)Provide financial support to developing countries to improve health infrastructure, strengthen medical services and improve health care. The World Bank also provides policy advice and technical support to the health departments of developing countries through data collection and research, helping them to formulate and implement effective health policies, plans and regulatory measures to improve the health of all people. The World Bank works with other international organizations, governments and non-governmental organizations to promote the global health governance agenda, promote cooperation and innovation in the health field, and help achieve the health goals of the United Nations Sustainable Development Goals.
Gates FoundationFounded in 2000, the vision is "a world where everyone has the opportunity to live a healthy and productive life". The Gates Foundation promotes development and improvement in the health sector through funding, resources and partnerships. New partnerships are encouraged to ensure that shared resources can bring the greatest benefits to the widest range of people. The Gates Foundation supports the creation of innovative cooperation mechanisms such as the Global Vaccine Alliance (Gavi), the Coalition for Epidemic Preparedness Innovations (CEPI), and the Child Health and Mortality Prevention Monitoring Network (CHAMPS) covering all of Africa, playing an important role in improving global health and achieving healthy sustainable development. In January 2024, against the backdrop of a global economic downturn, the Gates Foundation pledged to increase its annual budget to US$8.6 billion.
Global Fund to Fight AIDS, Tuberculosis and Malaria (the Global Fund)Founded in 2002, the Global Fund is a network of partners composed of governments, non-governmental organizations, the private sector and charities. Its mission is to accelerate progress in global health by raising funds and providing support, especially in the fight against major infectious diseases such as AIDS, tuberculosis and malaria. The Global Fund invests more than US$5 billion each year to defeat HIV, tuberculosis and malaria, ensuring a healthier, safer and more equitable future for all. The Global Fund plays an important role in reducing the spread of infectious diseases and improving the level of health services, and has made positive contributions to global health governance and health equity.
 (GAVI/Photo)
(GAVI/Photo)
Global Vaccine Alliance (Gavi)Founded in 2000, GAVI aims to save lives, reduce poverty and protect the world from epidemics. The Global Vaccine Alliance promotes global vaccination programs through partnerships and resource integration with governments, non-governmental organizations, the private sector and international organizations to ensure that all children have access to the vaccination services they need for life, thereby reducing child mortality and improving global public health. As of 2022, GAVI has helped vaccinate more than 1 billion children in 78 low-income countries, preventing more than 17.3 million deaths from unvaccinated children.
In addition, the Joint United Nations Programme on HIV/AIDS (UNAIDS) plays a vital role in coordinating the global fight against AIDS and promoting prevention, treatment and support services, and the International Federation of Red Cross and Red Crescent Societies (IFRC) plays a vital role in providing assistance and support during health emergencies and disasters.
International treaties and agreements are the foundation of global health governance
International treaties and agreements in the health field, such as the International Health Regulations (IHR), are intended to help Member States prevent and respond to cross-border and global public health risks. They are binding on all WHO member states and are an important foundation for global health governance.
The International Health Regulations are the core document for preventing and responding to global pandemics.The International Health Regulations set standards for the World Health Organization and its member states to identify and respond to public health events, as well as to share relevant information with each other. The International Health Regulations require member states to report all serious public health emergencies of international concern to the WHO, and require member states to review and strengthen their own public health surveillance and response systems, and enhance their ability to respond to public health emergencies of international concern. However, according to the International Health Regulations, the WHO has no power to force member states to carry out work related to protecting global health security, and its ability to coordinate with governments is also limited. Therefore, the large number of recommendations and coordination work put forward by the WHO in responding to cross-border epidemics such as the Ebola virus and the new coronavirus mainly stop at technical guidance. During the COVID-19 pandemic, the efforts of the WHO and governments of various countries have failed to prevent the spread of the epidemic around the world. This year's World Health Assembly adopted an amendment to the International Health Regulations, introducing the definition of "pandemic emergencies" to ensure that all countries have established a comprehensive and sound public health system and strengthen the global ability to prevent, monitor and respond to public health emergencies such as pandemics.
The Pandemic Agreement aims to strengthen global preparedness and response to pandemics.The agreement was proposed by the European Union in 2019. The COVID-19 pandemic has killed more than 7 million people worldwide and exposed huge inequalities in access to vaccines and health services among different countries. The World Health Organization played a facilitating and coordinating role in the negotiations on the Pandemic Agreement. In December 2021, the World Health Assembly held its second special meeting since its establishment in 1948 and decided to establish an intergovernmental negotiating body. In October 2023, the WHO announced the proposed negotiating text of the Pandemic Agreement. In March 2024, the ninth meeting of the Intergovernmental Negotiating Body discussed all the terms of the draft agreement, including adequate funding for pandemic preparedness, fair access to required medical countermeasures during a pandemic, and strengthening of health human resources. Due to differences among countries on better sharing of technology and pathogens that cause the epidemic, the current World Health Assembly failed to adopt the Pandemic Agreement. Countries agreed to "complete the negotiations on the Pandemic Agreement within one year at the latest, and possibly in 2024."
Global health governance faces many challenges
For decades, the global health governance system has played an important role in responding to and solving health problems around the world. Countries around the world have made a series of important achievements in achieving Goal 3 of the United Nations Sustainable Development Goals, "Good Health and Well-being". Improvements in medical facilities, sanitary conditions and medical services have led to a continuous decline in child mortality and maternal and infant mortality worldwide, and significant progress has been made in the control of AIDS, tuberculosis and malaria. By providing better medical services and preventive measures, the spread and lethality of related diseases have been reduced. Many countries have worked hard to provide basic health care services such as vaccination, maternal and infant health care, and infectious disease control to ensure that people have access to necessary health care. Through publicity, education and policy interventions, some countries have successfully reduced smoking rates and alcohol abuse, thereby improving people's health. The 2023 WHO Results Report shows that the world has made progress in several key areas, including the number of people with improved health, universal health coverage and protection from health emergencies.
Despite the achievements, the world still faces major challenges in achieving the goal of "health and well-being". Globalization has further led to health problems transcending national borders, and the uneven development of health systems in some countries and regions has led to unfairness in the provision of health services. In responding to emerging infectious diseases and global health challenges, the global health governance structure faces challenges such as decentralized power, insufficient funding, coordination difficulties, and insufficient coordination and response capabilities.
 (Pixabay/Image)
(Pixabay/Image)
There are systemic problems in the global health governance system.Global health governance involves multiple actors, including governments, international organizations, non-governmental organizations, and the private sector. These actors act independently, which may lead to challenges in the coordination and decision-making of global health governance, duplication of work and coverage, and fragmentation of the coordination mechanism of health governance. The overall coordination mechanism in the field of global health governance lacks binding force, resulting in poor results in global health governance. For example, during the COVID-19 pandemic, although the World Health Organization played an active role in coordinating prevention and control, the attitudes, methods and measures of various countries in responding to the epidemic were different, making it difficult to form unified actions. The lack of binding force of the systematic coordination mechanism is not conducive to the overall advancement of global health governance.
Populism, unilateralism and power politics affect international cooperation.Populist tendencies may cause some countries to shift their domestic political focus inward, weakening support for international health cooperation, especially when priorities are high or during economic recessions. Unilateralist tendencies may cause some countries to take unilateral actions rather than address global health challenges through multilateral cooperation, weakening the role and authority of organizations such as the WHO and affecting their due role in global health governance. Power politics may cause some countries to try to dominate international affairs through tough measures rather than solving problems through cooperation and consultation, thus hindering cooperation and coordination in the field of international health.
Funding is insufficient and unevenly distributed.The global health governance structure faces the challenges of insufficient funding and uneven distribution. Some regions and countries have insufficient funding for health infrastructure construction, medical equipment procurement, and medical personnel training, which affects the quality and coverage of health services. The lack of long-term sustainable financial support for the health system has made it difficult for some countries to respond to sudden health crises and epidemics. As a professional agency of the United Nations responsible for health affairs, over-reliance on voluntary donations has also had a significant impact on the professionalism and independence of the WHO, making it difficult for the WHO to play a role in the areas and places where it is most needed. This is one of the biggest challenges facing the WHO and the root cause of many other problems of the WHO.
Health data is incomplete and information sharing is poor.There are currently many challenges in the collection and sharing of health data and information around the world. The inconsistent data collection standards and methods used by different countries, regions and institutions have resulted in a lack of consistency and comparability in global health data. Some countries or regions lack advanced information technology infrastructure and data management systems, which limits the ability to collect, store and share data. Concerns about personal privacy and data security may limit the sharing and openness of data. Some countries may restrict data sharing due to political considerations or cultural differences, resulting in obstructed information flow. The lack of comprehensive and accurate data support may affect the comprehensive assessment and monitoring of the global health situation, and lead to a lack of scientific basis for decision-making, affecting the rational allocation of resources and the effective formulation of health policies.
Strengthening and improving global health governance is essential
The COVID-19 pandemic highlights the importance of strengthening global health governance. Strengthening global health governance is an important measure to ensure global health security, promote fair and sustainable development, maintain global economic stability, and promote global cooperation and coordination. Improving global health governance, promoting fair distribution of health resources, and effectively responding to global health challenges such as pandemics and antibiotic resistance require joint efforts from all countries.
Strengthen coordination among global health governance entities.Governments, international organizations, non-governmental organizations, and the private sector are all important entities in global health governance. Among them, governments are the fundamental driving force for promoting global health governance, and the World Health Organization plays a leading and coordinating role in global health governance. Due to the imbalance of global economic development, there are huge differences in medical supplies and talent reserves between different countries and regions, which requires effective collaboration between different governance entities. Global epidemics such as the new coronavirus, Zika virus, and Ebola virus cannot be dealt with by each country alone, but must be dealt with through global cooperation. Establish international cooperation among governments, international organizations, non-governmental organizations, and the private sector, jointly participate in global health governance, establish regular communication and information sharing mechanisms, and achieve resource sharing and complementary advantages. For example, the opening of the World Health Data Center has simplified the procedures for member states to obtain health data and approve national estimates. Jointly formulate global health goals and strategies, establish a unified action framework, and ensure that the actions of all entities are in the same direction, so as to effectively and collaboratively promote global health governance.
 (WHO/Photo)
(WHO/Photo)
Support relevant international organizations to play their due role.As the world's largest international health organization and the United Nations professional agency responsible for health affairs, WHO has a major responsibility in solving global public health problems. Countries should promote policy coordination and consensus through dialogue, policy docking and cooperation projects, establish effective communication channels, and strengthen political support for WHO. Countries should also strengthen financial support for WHO to ensure that WHO can fulfill its duties and tasks. The 2023 WHO Results Report shows that member states have pledged to provide sustainable financial support to WHO, taking the approach of increasing assessed contributions to 50% of the initially approved 2022-2023 planning budget basic budget by the 2030-2031 biennium.
Linking health and wellness with other global agendas and actions.Agendas such as climate change, poverty, education and gender equality are closely related to health and hygiene. A healthy population is essential to achieving sustainable development, eradicating poverty, promoting peaceful and inclusive societies, and protecting the environment. For example, the resolution on health and climate change approved by the 77th World Health Assembly is a milestone. A strategic roundtable of global health leaders and experts was held during the assembly to shape the global health architecture to respond to climate change. By closely linking health and hygiene with other global agendas and actions, synergies can be achieved, sustainable development of global health governance can be promoted, the health of people in all countries can be improved, and comprehensive sustainable development can be achieved.
Increase financial support for global health and diversify funding sources.Advocate for governments, international organizations and private sector partners to increase financial support and reduce the dependence of global health institutions such as WHO on a single donor or funding stream to ensure that there are sufficient resources to effectively respond to health challenges. Prioritize the equitable distribution of funds to ensure that resources are allocated according to health needs and priorities and reduce the influence of political or economic factors. Strengthen long-term financial support commitments and improve the stability and predictability of funding for health projects to strengthen health systems, respond to health challenges and achieve sustainable health results. Through these measures, overcome funding challenges and build a more effective and sustainable global health system to meet the diverse and complex health needs of the global population.
References
https://www.who.int/news-room/spotlight/10-global-health-issues-to-track-in-2021
https://www.who.int/zh/news-room/spotlight/global-health-achievements2023
https://data.who.int/dashboards/covid19/deaths
https://www.ohchr.org/zh/human-rights/universaldeclaration/translations/chinese
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3983705/
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(22)02576-4/fulltex
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7127552/

All rights reserved, please indicate the source when citing.
